Advanced Practice Updates Newsletter and News
Our APP email distribution list is now easier to search in Outlook. Go to the Global Address List and search APP. APPEmailCommunicationList
DL_APPEmailCommunicationList@NJHealth.org
APP Town Hall - August 26, 2025
View the Meeting recording below:
Advanced Practice Council Meeting - August 7, 2025
View the Meeting recording below:
Annual Performance Evaluation Information
APP-Performance-Evaluation-guide.docx
Frequently Asked Questions (FAQs) About Office/Outpatient (O/O) Evaluation and Management (E/M) Visit Complexity Add-On HCPCS Code G2211 and Evaluation and Management Power Point
2025-EM-Powerpoint-handout.pdf
2025 Outpatient Cheat Sheet and Level of Service Speed Buttons
New APP Policy can be found in Power DMS
We have a new policy for all APP's: APP Workweek Expectations, in the link below. It can also be found in Power DMS from the Spyderweb.
CME Requirement Resources
Some of you are renewing your DEA license this month, and I’ve gotten some questions about the 8-hour opioid CME requirement associated with DEA licensure. If any of you haven’t yet gotten these hours done, I wanted to pass along some free resources that I found. There are plenty of others, but here are a couple to check out:
- AMA Ed Hub
- NEJM has a course called “Free DEA-Required 8-hour training” on their website:
https://pain-management-cme.nejm.org/
Advanced Practice Provider Job Description
The Advanced Practice Provider job description has been updated for all nurse practitioners, physician assistants, and clinical nurse specialist providers at National Jewish Health. This is a standardized job description that is intended to reflect the common job duties of APPs across the organization. Any specific Department/Division level responsibilities will be outlined separately based on the specialty practice.
Please see the job description link below.
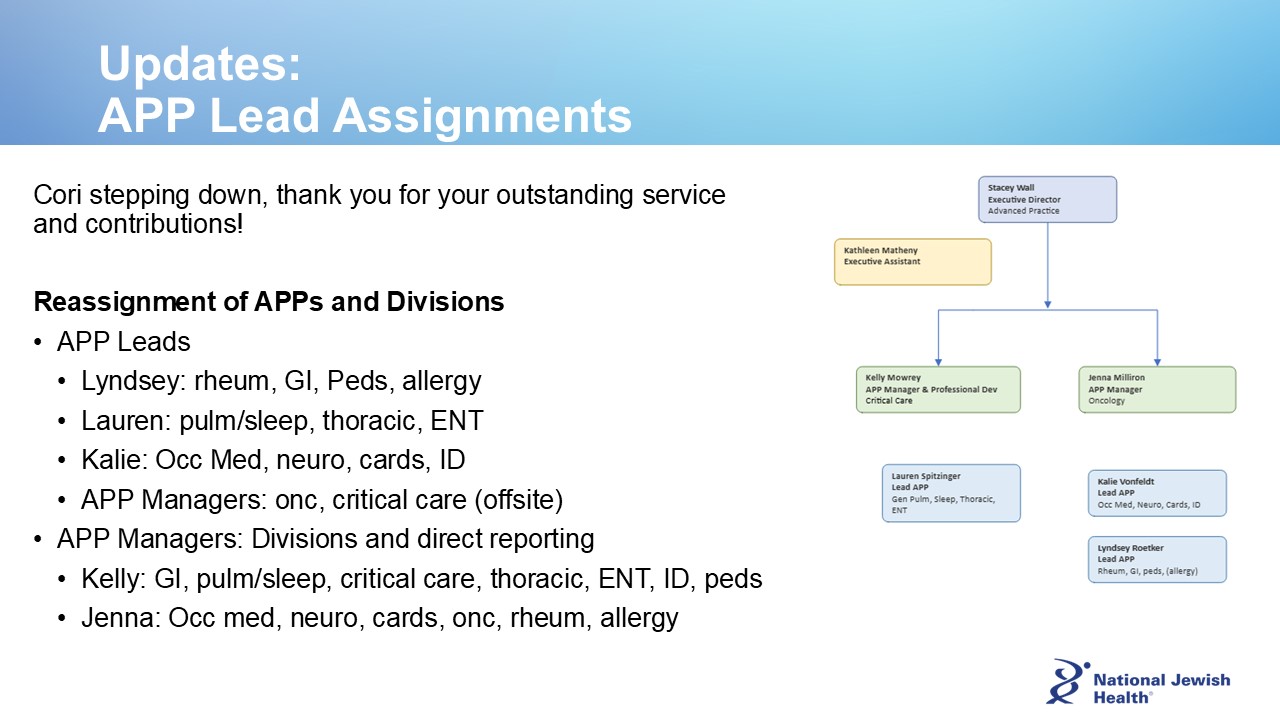
Changes to APP Structure in 2024
National Jewish Health implemented a new APP structure as of October 1, 2024. Changes include new APP Leadership roles, and transition of APP home Department and direct reporting. These changes are intended to provide support for APP growth and development, recognition for top of scope practice, alignment with faculty medical practice, and equity in professional expectations across the organization. Here is some additional background:
APP leadership roles include Leads and Managers. APP Leads serve as a resource and representative for groups of APPs, and function as a leadership partner for clinical leaders within the Division. APP Managers have direct supervisory responsibilities for APPs, oversee our APP Leads, and serve as a leadership partner with Division Chiefs.
APP reporting has transitioned to a matrixed structure. Direct reporting changed to the APP Manager who has supervisory responsibilities such as onboarding, Kronos timekeeping, and annual performance evaluation. Indirect reporting remains with the Division Chief (or designee) for oversight of clinical practice.
APP home department has transitioned from the Department of Nursing to the Departments of Medicine, Pediatrics, or Specialty Services and respective Division/Section.
APP Managers
 Jenna Milliron serves as the APP Manager for Neurology, Allergy & Immunology, Occupational Medicine, Gastroenterology, Cardiology, Pulmonary Hypertension, Metabolic Health, Rheumatology, Oncology, and Cystic Fibrosis. Jenna continues her clinical practice in Metabolic Health.
Jenna Milliron serves as the APP Manager for Neurology, Allergy & Immunology, Occupational Medicine, Gastroenterology, Cardiology, Pulmonary Hypertension, Metabolic Health, Rheumatology, Oncology, and Cystic Fibrosis. Jenna continues her clinical practice in Metabolic Health.
 Kelly Mowrey serves as the APP Manager for Pulmonary & Critical Care, Sleep Medicine, Otolaryngology, Thoracic Surgery, Anesthesiology, Infectious Disease, and Pediatrics. Kelly has additional responsibilities for developing programs to support APP education and professional growth. Kelly practices clinically in Interventional Pulmonology.
Kelly Mowrey serves as the APP Manager for Pulmonary & Critical Care, Sleep Medicine, Otolaryngology, Thoracic Surgery, Anesthesiology, Infectious Disease, and Pediatrics. Kelly has additional responsibilities for developing programs to support APP education and professional growth. Kelly practices clinically in Interventional Pulmonology.
APP Leads
- Kalie Vonfeldt: Neurology, Allergy Immunology, Occupational Medicine, Gastroenterology, Cystic Fibrosis
- Lauren Spitzinger: General Pulmonary, Critical Care
- Lyndsey Roetker: Rheumatology, Oncology, Cardiology, Pulmonary Hypertension, & Metabolic Health
- Anesthesiology (under recruitment): Minimally Invasive Diagnostic Center CRNA practice
AP Structure
Download the December 2023 issue.
Download the September 2023 issue.
News for Advanced Practice Providers
 SB23-083 Physician Assistant Collaboration Requirements
SB23-083 Physician Assistant Collaboration Requirements
The Colorado Department of Regulatory Agencies (DORA) and the Colorado Medical Board finalized rulemaking for SB23-083. Rule 1.15 (formally Rule 400) is finalized and effective as of August 17, 2023.
The Colorado Medical Board finalized rules on August 17th to implement changes set forth in SB23-083: Physician Assistant (PA) Collaboration Requirements. This new law removes the requirement that a physician assistant be supervised by a physician or podiatrist except in certain circumstances.
These revisions can now be found in Medical Board Rule 1.15. The Board also has developed a Frequently Asked Questions document that may clarify any uncertainty created by these changes.
Please review these documents to familiarize yourself with the nature of collaborative agreements, and when supervising agreements are instead appropriate.
Do you need a Collaborative Agreement? Sample Collaborative Agreement
Need more information? FAQ PA Collaboration
Want to learn more about Collaborative Practice? Attend CAPA's PA Professional Day
Colorado Board of Nursing Stakeholder Meeting

The Colorado Board of Nursing (BON) held a virtual Stakeholder Meeting on September 8, 2023, to receive feedback on several bills and proposed changes to Rule 1.15 Rules and Regulations for Prescriptive Authority for Advanced Practice Registered Nurses. The Permanent Rulemaking Hearing will be held on Wednesday, October 25, 2023, at 9:30 a.m. (MDT).
The Colorado Nurses Association and Colorado Society of Advanced Practice Nurses have been connecting with advocates, and encourage individuals to correspond with the BON directly about how these proposed changes will affect their practice. The proposed changes will have the greatest impact on Family Nurse Practitioners (FNP). Please see the outline below for specific proposed changes as well as the link to the full draft rule.
To obtain Full Prescriptive Authority in a Population Focus, the following shall be documented as part of the required 750 hours of Mentorship:
Family and Individuals Across the Lifespan:
- Primary Care - 350 Clinical Hours with a corresponding mentor
- Pediatrics - 150 Clinical Hours with a corresponding mentor
- Adult - 150 Clinical Hours with a corresponding mentor
- Geriatric - 50 Clinical Hours with a corresponding mentor
- Women’s Health - 50 Clinical Hours with a corresponding mentor
Written comments may be submitted online here or emailed to dora_dpo_rulemaking@state.co.us


