Advance Directives
As part of the action plan, talk with your health care provider, caregiver and family about what treatment you desire if you should become seriously ill and unable to express your wishes.
An advance directive is a legal form that states what medical decisions are made and who will make them when an individual is not able to respond to a medical team or is unable to make his or her own decisions. These decisions can include if a person wishes to be on life support, receive artificial nutrition (tube feeding) or receive cardiopulmonary resuscitation (CPR), among other medically-based legal decisions. A living will is one form of an advance directive.
Transcript
Advance care planning is important because it gives patients and families an opportunity talk about an emergency before an emergency happens.
It’s a lot easier to make health care decisions at a quiet time around the kitchen table rather than when the ambulance crew is in the living room.
An advance directive is a document that offers guidelines regarding a patient’s health care wishes.
For example, who the decision maker should be, if the patient is not able to make his or her own health care decisions.
Also, what health care treatments a patient may or may not want.
An advance directive is a modern version of a living will that is a little bit more general.
For example, it identifies a health care decision maker for the person and offers a few guidelines, but is not detailed in the way a living will may be a detailed legal document.
An advance directive goes into effect at the time the patient is no longer able to answer questions regarding his or her health care.
It’s important to discuss the advance directive with the medical durable power of attorney, the person who is going to be making health care decisions for you while you are unable to speak for yourself.
It would be important to share your advance directive with your physician and then your specialist who you see most often.
These are among the physicians most likely to receive a call from the emergency room where the ER staff is looking for information on the patient.
A patient does not have to have a terminal illness in order to complete an advance directive.
In fact, all people should have an advance directive.
We never know what’s going to happen to us, it’s always a good idea to have a document and make sure we have some guidelines to offer family and friends when we are hospitalized and unable to speak for ourselves.
How is an advance directive different than my will?
An advance directive only includes medical decisions and whom you designate to make medical decisions. A will may discuss assets and distribution of these assets. Some people may have a will that also includes a section on their advance directives.
When should I complete an advance directive?
An advance directive should be completed at all stages of life. We do not know when we may not be able to make our own decisions. Car accidents, accidental injuries, symptoms of a chronic disease and infections are just some of the reasons you may not be able to make your own medical decisions.
How can an advance directive help?
Every state has different laws about who makes decisions and what decisions are made. Having an advance directive in place allows you to have a say in what decisions are made for you. For example, in Colorado, advance directives include a living will, a medical durable power of attorney, a CPR directive and others.
An advance directive also can help the people you have selected (or whom the state selects if you have not designated anyone) in making decisions. It can be a very difficult decision to take someone off life support if that person never talked about dying, especially if they feel “they have so much life to live.” It also can assists families who have different opinions on what actions should be taken. Families often disagree on what care should be provided when someone cannot speak for himself or herself. An advance directive makes those wishes clear.
What’s included in advance directives?
Advance directives comes in many forms, but generally advance directives will include:
Who you want to make medical decisions for you, including a primary and backup decision-maker
If you want to be on life support if you are deemed brain dead or in a coma
If you want to have tube feedings or artificial nutrition
If you do or do not want cardiopulmonary resuscitation (CPR)
If you would like to be in a nursing home or moved to another state.
Some forms also include if you prefer burial versus cremation, what you would like a funeral service to include, and what you want loved ones to know after you have died.
Advance directives can include as little or as much as you want them to include.
When is an advance directive activated?
An advance directive is only activated when you are deemed unable to make your own medical decisions. This can be determined by a doctor while in an emergency room and in some cases by a judge.
If you are able to respond to a medical provider and are oriented to person, place and time, an advance directive will not be active. This means the people you have designated to make medical decisions cannot make them if you are still able to speak for yourself.
 How can I complete an advance directive?
How can I complete an advance directive?
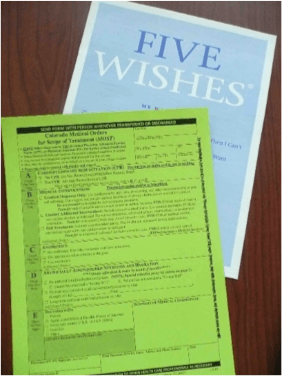
You can make an advance directive by yourself or with the assistance of a lawyer. Some forms have been made to assist you in completing an advance directive. Examples of advance directive forms include Five Wishes® and Medical Orders for Scope of Treatment (MOST). When using a form, you will need to verify if it is legal in your state. Most states have online advance directive forms available for download.
Where should I keep my completed advance directives?
Your advance directives should be kept in a safe and secure location. It should be a location that the people whom you have designated to make your decisions have access to. You may also provide copies to your primary care doctor, local hospitals (even if you have not been a patient there) and any specialists you may see. You may also choose to provide a copy to your decision-makers and your attorney.
What if I want to change my advance directive?
As long as you are still deemed able to make your own decisions, your advance directive can be changed at any point. If you want to make changes, check with your state laws for specific requirements. However, in most states, you would need to write VOID across any copies of a current advance directive or destroy any copies. The advance directive that will be deemed accurate is the most recent completed form, unless it is determined by a judge that those changes were made after you lost ability to make your own decisions.
