New Diagnostic Criteria Proposed For Chronic Obstructive Pulmonary Disease (COPD)
New criteria could identify more patients in early stages of disease, promote better care and stimulate research to slow and prevent COPD
Denver, CO —
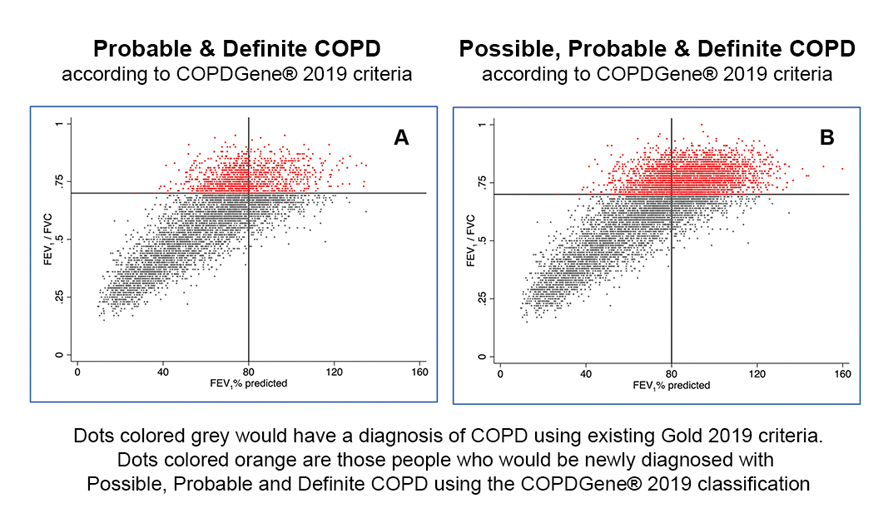
Researchers at National Jewish Health and dozens of leading institutions around the nation have proposed new criteria for diagnosing chronic obstructive pulmonary disease (COPD), the fourth leading cause of death in the United States. The proposal, published in Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation, expands diagnostic criteria from a single measure of lung function to include environmental exposure, symptoms, and abnormal CT scans. If used, the new diagnostic criteria could increase the number of patients diagnosed with COPD, by 15 percent to 36 percent, or about 2 million to 5 million people.
“Our proposed diagnostic criteria better capture the full spectrum of people suffering from COPD,” said James Crapo, MD, senior author on the paper. “This can lead to better care for patients and stimulate research to slow or stop progression of the disease or even prevent it.”
COPD is a progressive, complex combination of airway inflammatory disease, chronic bronchitis and emphysema. Smoking tobacco is the most common cause of COPD, although about 15 percent of COPD patients never smoked. Approximately 12 million people in the United States have been diagnosed with COPD, and many million more are thought to have undiagnosed COPD. Every year, about 120,000 people in the United States die of the COPD.
The researchers evaluated 8,784 smokers and former smokers enrolled in the COPDGene® study. At enrollment, the researchers documented patients’ environmental exposures (smoking), symptoms (shortness of breath, chronic cough and phlegm), structural abnormalities on CT scans (emphysema, gas-trapping and airway wall thickness) and lung function or spirometry (total volume of air exhaled from the lungs, and the volume of air exhaled in one second). They then correlated those measures with mortality and loss of lung function five years later and compared them with smokers with none of the other criteria.
All patients met one of the criteria: smoking history. Those meeting either one, two or three additional criteria all had increased risks of losing significant lung function in five years or dying.
Smokers meeting one of the other three criteria were designated as having Possible COPD. Their risk of losing significant lung function was 26 percent greater than smokers meeting no additional criteria, and a 28 percent higher chance of dying within five years.
Smokers who met two of the three additional criteria were designated as having Probable COPD. They had an 88 percent greater chance of losing significant lung function and an 89 percent greater chance of dying.
Those with all four diagnostic criteria were designated as having Definite COPD. They had a 188 percent greater chance of losing significant lung function over five years and more than 5 times the risk of dying.
| Proposed COPD Diagnostic Criteria: 1) Smoking History 2) Symptoms 3) Impaired Lung Function 4) Abnormal CT Scan |
Odds ratio of significant lung function loss (FEV1 loss >350 ml) |
Hazard ratio for all cause mortality |
| Smokers | 1.0 | 1.0 |
| Smokers with one additional criterion | 1.26 | 1.28 |
| Smokers with two additional criteria | 1.88 | 1.89 |
| Smokers with all three additional criteria | 2.88 | 5.21 |
“If we diagnose COPD based only on impaired lung function, then we miss many patients in the early stages of the disease,” said Dr. Crapo, who is also co-principal investigator of COPDGene®. “While some physicians do empirically treat patients with symptoms, many patients are not getting therapy that can improve their symptoms, their quality of life, and might extend their lives.
“Right now people who do not meet the current diagnostic criteria for COPD are not included in clinical trials of experimental COPD therapies. Our proposed diagnostic criteria could open clinical trials to these people, stimulate important research of potential therapies to slow, stop or even prevent progression of the disease.”
National Jewish Health is the leading respiratory hospital in the nation delivering excellence in multispecialty care and world class research. Founded in 1899 as a nonprofit hospital, National Jewish Health today is the only facility in the world dedicated exclusively to groundbreaking medical research and treatment of children and adults with respiratory, cardiac, immune and related disorders. Patients and families come to National Jewish Health from around the world to receive cutting-edge, comprehensive, coordinated care. To learn more, visit njhealth.org or the media resources page.
Media Resources
We have many faculty members, from bench scientists to clinicians, who can speak on almost any aspect of respiratory, immune, cardiac and gastrointestinal disease as well as lung cancer and basic immunology.
Media Contacts
Our team is available to arrange interviews, discuss events and story ideas.
- Jessica Berry
303.398.1082 office
303.807.9491 mobile
berryj@njhealth.org - Adam Dormuth
303.398.1002 office
970.222.5034 mobile
dormutha@njhealth.org
