This information was reviewed and approved by Patrick S. Hume, MD, PhD (7/1/2024).
- Do not delete this
What is Chronic Obstructive Pulmonary Disease?
Chronic obstructive pulmonary disease (COPD) affects more than 14 million people in the United States. “Chronic" means long term. "Obstructive" means it is hard to get air out of the lungs. The most familiar diseases in this group are emphysema and chronic bronchitis. A person with COPD may have emphysema, chronic bronchitis, or both. COPD shares characteristics of asthma.
COPD is chronic obstructive pulmonary disease. Chronic means the condition is going to be there, it's been there for a long time, it's going to be there for a long time, but the good news is that COPD is treatable in addition to being long standing. Obstructive refers to the fact that the breathing test has a certain kind of abnormality with air flow limitation. Pulmonary disease, it's a problem of the lungs inside the chest.
Shortness of breath, cough and phlegm are the major symptoms of COPD that drives patients to come see their physician. Shortness of breath is sometimes first recognized as inability to do what you normally can do. In addition, many patients have what's called exacerbations. That means some acute respiratory event which is associated with more shortness of breath, more cough, more phlegm, those exacerbations are very important and need to be treated appropriately and rapidly.
The most important and common diagnostic test for COPD is a breathing test. The name of that breathing test is spirometry, but it's pretty simple. It requires you to take a deep breath in and blow it out as hard and fast as you can. With that test, we find out that the air passages are narrow and that's sort of the classic definition of COPD along with symptoms. In addition, there's some other tests that people sometimes have. They may go in and have a CAT scan of their chest because they have some other respiratory complaint and one finds emphysema on their chest x-ray. Breathing tests and x-rays are the most common ways we diagnose COPD.
The important thing that people should know about COPD is it's treatable. Think about what symptoms you have as an individual. If you have shortness of breath, we have lots of treatments for that. One of the important treatments is actually a non-medical treatment, at least a non-medication treatment and that's exercise. If you exercise regularly, you'll be able to do more before you get out of breath. A regular exercise program is sometimes started as what's called pulmonary rehabilitation, a program of exercise and education that allows people to do more, be more active through a regular exercise program that's targeted for them. In addition, we also have treatments related to medications that one needs to breathe in. There are a lot of different kinds and classes of medications that help people be less short of breath when they have COPD by using these medications on a regular basis.
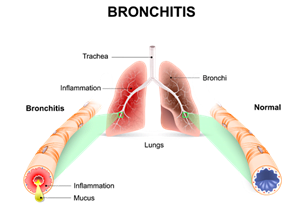
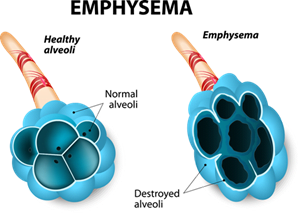
With COPD, the air sacs, also called alveoli, and the airways have been damaged, most often by cigarette smoking or poor air quality. In healthy lungs, the air sacs or alveoli look like a bunch of grapes. In emphysema, the walls of the alveoli are partially destroyed. This results in a smaller total number of alveoli in the lungs. Fewer air sacs mean that the lungs are not able to absorb oxygen into the bloodstream or expel carbon dioxide. The airways also may collapse a little.
In a healthy airway, air moves in and out of the middle of the airway. In chronic bronchitis, the airway walls are swollen and produce more mucus. In chronic bronchitis, a person has a chronic productive cough. This is often due to cigarette smoking.
COPD was once seen as a disease with a hopeless prognosis, but is now known to be very treatable. Early diagnosis and treatment can enable people with COPD to take charge of their breathing and regain control of their lives.
COPD Causes
- About 1-2% of COPD cases are caused by genetic-based deficiencies in an enzyme called alpha-1 antitrypsin. In these people, COPD may begin at a young age.
- Being exposed to secondhand smoke (either cigarette smoke or wood smoke in developing countries) for long periods of time, including during childhood, is also known to cause COPD.
- Long-term exposure to air pollution or chemical fumes can also cause COPD.
- More than 80% of COPD cases in the U.S. are caused by smoking cigarettes.
- Other cases are caused by significant exposure to various types of dust, such as coal, grain or wood, or by recurrent or significant lung infections in infancy and early childhood.
- People with COPD also can have exacerbations (flare-ups), which are periods of restricted breathing that can be severe. COPD exacerbation is most often caused by an infection, either in the lungs or the body, which causes inflammation in the lungs. COPD exacerbations can also be caused by a person with COPD continuing to smoke tobacco.
- Some people who have asthma can develop COPD.
COPD is not contagious. Most people who have the disease are at least 40 years old when symptoms begin. COPD is the fifth leading cause of death in the U.S. Its prevalence is declining in men, many of whom quit smoking over the past several decades. Its prevalence is increasing in women, reflecting the fact that more women began to smoke at about the same time many men began to quit. The lag time between when a person began to smoke and the development of COPD is 10 or more years.
Signs and Symptoms
The earliest symptom of COPD is more shortness of breath with strenuous activity than what would normally be reported from someone of a similar age. Many people do not realize this and may simply reduce the amount of activity they do. Later symptoms with COPD include shortness of breath with less activity.
Sometimes it is hard to know what to do when your symptoms change or worsen. It is normal to have good and bad days. COPD flare-ups, called COPD exacerbations, are when symptoms get worse. COPD flare-ups also may be called a chest cold or bronchitis. Knowing when symptoms are changing is helpful, so that treatment and other interventions can begin quickly.
Early Warning Signs
Early symptoms or warning signs of a COPD flare-up or exacerbation are unique to each person and may be the same, similar or different with each episode in the same person. Usually, you will be the best person to know if you are having trouble breathing.
However, some changes are more likely to be noticed by other people. It is important to share this information with your family and those close to you, since a change or increase in the symptoms you have may be the only early warning sign.
You may notice one or more of the following:
- A change in sputum color to yellow or green or the presence of blood in the sputum
- A cough and/or wheezing
- A general feeling of ill health
- Forgetfulness, confusion, slurring of speech and sleepiness
- Increased feeling of fatigue and lack of energy that is persistent
- An increase in the amount of sputum produced
- An increase in the severity of shortness of breath
- Trouble sleeping
- Using more pillows or sleeping in a chair instead of a bed to avoid shortness of breath
Things That Make Symptoms Worse
There are many effective measures you can perform at home to treat signs and symptoms. There also are actions that should be avoided:
- Increasing the liter flow of prescribed oxygen
- Smoking
- Taking codeine or any other cough suppressant
- Using over-the-counter nasal sprays for more than three days
- Waiting any longer than 24 hours to contact your health care provider if symptoms continue
Diagnosis
The first step in a COPD diagnosis is a thorough evaluation by an experienced doctor. A specialist who often sees people with COPD is a pulmonologist.
Your doctor will conduct a complete physical exam and ask you questions about your lifestyle, including your family, your job, your habits, your hobbies, your current medications and your symptoms.
Your doctor may have you do a number of tests to evaluate your breathing, lungs and other aspects of your health. There are other diseases and disorders that may be confused with COPD, but also may be seen with COPD and lead to a COPD diagnosis. These tests will help determine the right diagnosis and the best treatment plan for you.
Lung Cancer Screening
COPD can increase the risk of lung cancer. When being diagnosed for COPD, your doctor also may screen you for lung cancer. A lung cancer screening will look for signs of lung cancer before you have symptoms. Early treatment of lung cancer is essential for ensuring the best possible outcome.
Breathing and Exercise Testing
There are different types of breathing and exercise tests that can be under the coaching of a technician, using specialized equipment. The results of can help your doctor find the best treatment plan for you and monitor the progression of COPD.
Bronchial provocation test: The bronchial provocation test evaluates how sensitive the airways in your lungs are. A spirometry breathing test is done before and after you inhale a spray such as methacholine. The spirometry results are compared before and after you inhale the spray to see what changes there are in your breathing.
Cardiac stress test: This test may show evidence of blockages in the heart arteries when the heart is stressed. Medicine or exercise may be used during a cardiac stress test. Either will temporarily increase your heart rate and/or open up (dilate) the heart arteries.
Complete pulmonary function tests: Pulmonary function tests provide a more in-depth measure how well you are breathing, as they combine spirometry with measurements of lung volumes and ability of the lung to transfer inhaled gases from the air into the bloodstream. The results of pulmonary function testing can help your doctor find out more about the kind of COPD you have and how severe it is.
Exercise for desaturation testing: The exercise for desaturation test evaluates if you may benefit from supplemental oxygen at rest and during exercise.
Exercise tolerance testing: The exercise tolerance test evaluates the level of activity you can perform. It also evaluates your oxygen needs when you exercise and how your lungs and heart are responding to exercise. The results of the test can help our doctor determine why you experience shortness of breath during exercise.
Pulse oximetry: Pulse oximetry can measure the oxygen level in your finger. It can be done when you are resting, walking, and sleeping. This test evaluates if you may benefit from supplemental oxygen at rest or during exercise. If the oxygen gets low during sleep, you may be referred for a more detailed sleep testing.
Spirometry: A spirometry test measures airflow in and out of the lungs. This indicates whether or not there is airway narrowing that obstructs the flow of air in and out of the lungs. Spirometry test results are useful in making the diagnosis of a class of lung disorders. Even more important, yearly spirometry measurements help to detect lung disease at an early stage when lifestyle changes and treatment may help forestall future problems.
Imaging Tests
Abdominal ultrasound: An abdominal ultrasound (sound waves) can be used to look at organs, soft tissue and blood vessels within the abdomen.
Bone scan: A bone scan is a test that can identify bone that is diseased or injured. Normally, bone absorbs nutrients that are the building blocks of bone formation. If bone is diseased or injured, nutrients are absorbed differently. The bone scan takes pictures of this process. A bone scan can detect bone disease or injury that may not be seen with a traditional x-ray.
CT scan of the chest: A CT or CAT scan is a shortened name for computerized tomography. During a CT scan of the chest, detailed pictures are taken of cross sections or slices of the thoracic structures in your body. Thoracic structures include your lungs, heart and the bones around these areas. Sometimes intravenous contrast is administered to better see the blood vessels in the lung.
Echocardiogram: An echocardiogram (ECG or EKG) is an ultrasound of the heart. The ultrasound shows the structures and functions of the heart muscle and heart valves from different angles. It does this by using sound waves.
X-rays: X-rays can show irregularities or damage in the lungs caused by COPD and other acute and chronic lung diseases. You doctor may verify a diagnosis, or evaluate what other diseases or conditions may be present with other tests.
Lab Tests
Arterial blood gas testing: Arterial blood gas is a blood test ordered by your physician to evaluate measurements of oxygen level, carbon dioxide (effectiveness of respiration) and several other parameters. Generally, it is used when your physician needs to evaluate the effectiveness of your breathing.
Mucus culture: Some kinds of bacteria like to live in the mucus produced in the sinuses and airways of the lungs. A culture of this mucus can help identify an infection. Lung and/or sinus infections can complicate and/or mimic some symptoms of COPD.
Diagnostic Procedures
Bronchoscopy: A bronchoscopy allows the doctor to look inside the airways in the lungs. The bronchoscopy can be recorded to look at later. Your doctor also may do a lavage, which involves putting a small amount of fluid into the airways. The fluid is then pulled out with cells from the airways of your lungs. A biopsy of the airway also may be done, where a small amount of the tissue is taken from the lining of the lung. The cells and tissue can be studied closely to help determine your diagnosis and the best treatment for you.
pH impedance study: A pH impedance study measures the amount of gastroesophageal reflux you have. Gastroesophageal reflux is the backward flow or reflux of food and acid from the stomach into the esophagus. The esophagus is the tube that takes food from your mouth into your stomach. A pH impedance study will help identify if you have increased amounts of reflux and if it is causing you to have more exacerbations or flare-ups of your COPD.
Treatment
There are a variety of treatments that can help people with COPD to lead active full lives. People with COPD should become active in the treatment and management of their disease. Participating in your treatment plan will help you and your family take charge of your breathing. Talk with your health care provider about a treatment that will help you achieve your goals.
Medications
Your doctor may prescribe medicine to control the symptoms of COPD. Most people with COPD take long-acting medicine every day to help shortness of breath. In addition, short-acting medicine is used on an only-when-needed basis to decrease shortness of breath. For many, a combination of medicines is prescribed.
The important thing to remember is that there is no "best" drug regimen. Your medicine is individualized based on your symptoms and needs. Monitoring your COPD and working with your health care provider on an ongoing basis is the best way to ensure that your medicine is right for you.
Here are the types of medications generally prescribed for people with COPD:
- Antibiotics: Antibiotics can help treat bacterial infections in the lungs and prevent them from growing.
- Bronchodilators: Bronchodilators help open the airways in the lungs by relaxing smooth muscle around the airways. Bronchodilator medication can be short or long acting. There are different types of short or long acting bronchodilators that work in different ways.
- Anti-Inflammatory Medications: Anti-inflammatory medication helps reduce and prevent inflammation inside the airways.
- Steroid Pills: Steroid pills are very effective at reducing swelling and mucus production in the airways. They also help other quick-relief medication work better.
Talk to your doctor about managing your medications.
Immunizations
Immunizations for influenza and other respiratory infections may reduce your risk of infection and exacerbations.
- Make sure you get the COVID-19 vaccine annually.
- If you’re over 60, it’s recommended that you receive the RSV vaccine.
- Get the pneumococcal conjugate vaccine (PCV20) if you have not already received a pneumococcal vaccination.
Oxygen Therapy
Some people with COPD may benefit from oxygen therapy. Oxygen therapy is used to ensure there is enough oxygen in the blood to provide for the body's needs.
Lifestyle Management
Lifestyle changes can be an effective and simple way to improve your COPD symptoms. Talk to your doctor about the daily routines that can have a major impact on your COPD. Here are a few habits that can have a positive effect.
Avoid infection
Although it is important to take preventive measures to avoid lung infections, you do not need to isolate yourself from other people. There is no guaranteed way to prevent infections. However, if you are proactive with your vaccines, wash your hands thoroughly and frequently (with soap) and are aware of your surroundings, then you will increase your chances of living an infection-free life. Learn best practices for stopping germs.
Become more active
An exercise program is another very important step in managing COPD. It is common for people with lung disease to limit physical activities because they are afraid of becoming short of breath. However, regular exercise can improve your heart, lungs and muscles, and it can help you breathe easier and feel better. Many people with COPD enjoy walking, water aerobics and riding a stationary bike. Talk to your doctor about breathing techniques that can help you when you’re active.
Decrease anxiety or stress
Patients with COPD may experience increased episodes of panic and anxiety. This response is common and does not mean that there is something wrong with you mentally or emotionally. With help from your doctor, there are a number of things you can do to "reset" your suffocation alarm and your feelings of anxiety.
Decreasing shortness of breath
It is helpful to use effective breathing techniques with exercise to minimize shortness of breath and assure adequate oxygen to your working muscles. These breathing exercises have the added benefit of helping you relax when you are anxious or stressed. Three types or breathing techniques are pursed lip breathing, coordinated breathing with exercise and diaphragmatic breathing. Diaphragmatic breathing also is sometimes called “belly breathing.” Talk to your doctor to discuss specific ways you can incorporate breathing techniques to help with your shortness of breath.
Learn more about COPD
Learn about patient education classes and support groups at National Jewish Health.
Procedures
Testing can help your health care provider determine whether lung volume reduction surgery (LVRS) and bronchoscopic lung volume reduction (bLVR) may be beneficial for you.
LVRS and bLVR Surgeries
LVRS and bLVR are considered for people who are found to have moderate to severe emphysema on a chest CT scan.
There are often portions of the lung tissue that are more diseased than other portions. LVRS removes up to 20-30% of the most diseased tissue from the lungs at one time. BLVR removes the diseased section by using valves that collapse the disease portion. Removing some of the emphysema helps the healthier areas of the lungs and muscles to function better. People often are able to exercise more and feel less short of breath following lung volume reduction.
Lung volume reduction surgery is considered for adults with certain patterns of severe emphysema. Specific tests are done to determine if lung volume reduction surgery is recommended. These tests include breathing tests, a chest CT scan, an arterial blood gas (ABG), a lung perfusion study and exercise tests.
If LVRS or bLVR are considered a person must have quit smoking for at least six month and participate in a pulmonary rehabilitation program before and after the surgery.
People who benefit from LVRS have severe emphysema with certain patterns of emphysema on a chest CT scan, particularly those with more emphysema in the upper lobes and a low exercise tolerance. Other benefits of LVRS include less shortness of breath, improved quality of life and a longer life.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a program for people with chronic lung diseases like COPD, emphysema and chronic bronchitis. It will allow you to be as active as possible.
Pulmonary rehab is aimed to improve quality of life by:
- Decreasing respiratory symptoms and complications
- Encouraging self-management and control over daily functioning
- Improving physical conditioning and exercise performance
- Improving emotional well-being
- Reducing hospitalizations
Most pulmonary rehab programs include:
- Exercise
- Breathing exercises
- Education
- Emotional support
- Medical management
- Nutrition counseling
COPD Clinical Trials
Clinical trials help determine new treatment options for diseases and conditions. Patients with COPD have access to clinical trials and should speak with their doctor to determine what trials might work best for them.
See a Specialist
It’s important to be evaluated by a pulmonologist who specializes in COPD if you or a loved one:
- Has symptoms of COPD
- Has a history of smoking
- Would like strategies to help improve your current treatment of COPD
At National Jewish Health in Denver, Colorado, we have one of the world’s leading COPD treatment programs. Learn more about our program or use the button below to make an appointment.
 Clinical Trials
Clinical Trials
For more than 100 years, National Jewish Health has been committed to finding new treatments and cures for diseases. Search our clinical trials.
