Newsroom
Our public affairs team works with news outlets from all over the nation to bring you the latest health care news and information.
National Jewish Health has pulmonologists, infectious disease specialists and intensive care experts informed and available to talk about COVID-19 coronavirus. Visit our Coronavirus information site.
For More Information
Director, Media Relations & Communications
303.398.1082 office
303.807.9491 mobile
berryj@njhealth.org
Recent Press Releases

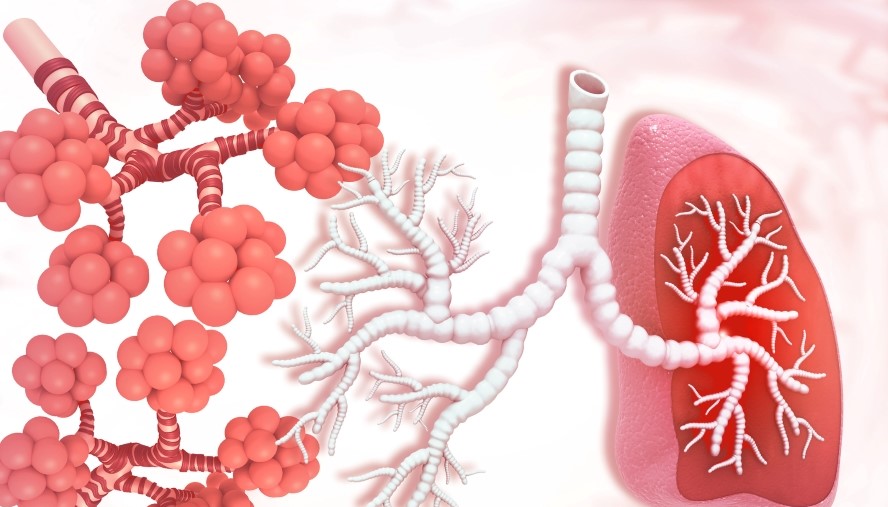
National Jewish Health Researchers Coin New Term ‘Silicosarcoidosis’ to Define Distinct Occupational Lung Disease
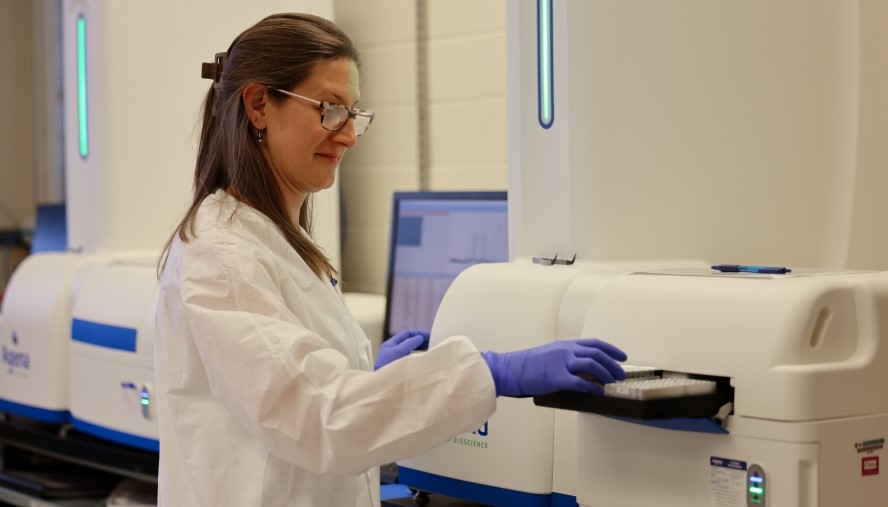
National Jewish Health Develops Advanced Molecular Test to Improve Diagnosis of a Genetic Form of COPD

New Research Evaluates the Ability of Patients with Adrenal Crisis to Complete Emergency Cortisol Injections
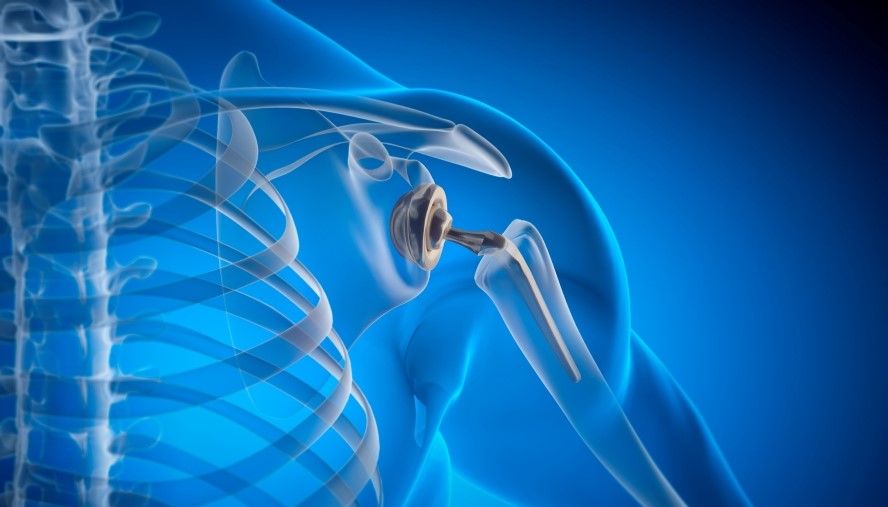
National Jewish Health Led Research Offers Key Insights into Metal Allergies and Impact on Surgical Outcomes for Patients

Lion King-Themed Beaux Arts Ball Raises $2 Million to Benefit National Jewish Health

New Study Identifies Genetic Links between Asthma, Respiratory Inhalers and Air Pollution

National Jewish Health Welcomes Pediatric Pulmonologist Dr. Alicia Della Volpe

Research Shows Positive Impact of CFTR Modulators on Pregnancy Outcomes in People with Cystic Fibrosis

Dr. Daniel Groves Joins National Jewish Health Cardiology Team

New Study Links Dust Storms to Increased Emergency Department Visits in the U.S. Southwest

“Forever Young – A Tribute to Andrew Young” Gala to Raise Critical Funds for Lifesaving Care and Research Planned for May 12, 2025

Doctors warn air pollution not only affects the lungs, but also contribute to heart disease

National Jewish Health Launches Groundbreaking Study on Food Allergies

Derek Abbott, MD, PhD, Named Cecil and Ida Green Chair of Department of Immunology and Genomic Medicine at National Jewish Health

Wendy M. Siegel Honored at the 56th Real Estate and Construction Industries Dinner Dance Gala in New York
New Study Shows Role of Macrophages Misunderstood in Fibrosis

Dr. Harry Fischer Joins the Rheumatology Team at National Jewish Health

Research Shows Medication Effective in Treatment of Children with Atopic Dermatitis

Dr. Girish Paranjape Joins the National Jewish Health Concierge Medicine Program in the Wellness and Prevention Clinics

Rev the Runway Raises Nearly $385,000 for National Jewish Health

Holiday Gatherings Can Be Stressful and Dangerous for Kids with Food Allergies

Researchers Identify a Protein Involved in Mucus-Related Airway Obstruction in People with Asthma
Dr. Kathleen Yan Joins National Jewish Health Gastroenterology Team

Dr. Mark Mallozzi Joins National Jewish Health Pulmonology Team

Dr. John Goff Joins National Jewish Health Gastroenterology Team

Steps to Improve Indoor Air Quality Should Be on Every Parent’s Child-Proofing Checklist

Rev the Runway Aspen Event Raises Nearly $530,000 Benefiting National Jewish Health

National Jewish Health Physicians Recognized as “Top Doctors”

Researchers Examine Respiratory Health Issues in Olympic Athletes

National Jewish Health Named a Top Hospital in Pulmonology by U.S. News & World Report

Night & Day Golf Classic Raises More Than $280,000 for Morgridge Academy

Potential of Inflammatory Biomarkers to Guide Treatment in Mild Asthma

Annual Black & White Ball Raises More than $440,000 to Benefit National Jewish Health

Researchers Evaluate Allergy Skin Test Responses in U.S. Asthma Population

Dr. Kevin Rurak Joins National Jewish Health Pulmonary Hypertension Team
Irina Petrache, MD, Appointed 2024-25 President of American Thoracic Society
Browse by year
Multimedia Story Assets
Upcoming Fundraising Events
Upcoming Education Events
April
May
Managing Upper and Lower Airway Diseases: The Role of Epithelial-Driven Inflammation
6:30PM
Marriott San Francisco Marquis - Golden Gate Ballroom A/B
780 Mission St, San Francisco, California 94103June
Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The New Era of Prevention Sponsors and Exhibitors
7:00AM
Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The New Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The Next Era of Prevention (Hybrid Event)
7:00AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206Improving Cardiovascular Outcomes: The New Era of Prevention (Hybrid Event)
7:05AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206September
2025 NTM & Bronchiectasis Conference for Healthcare Providers (Hybrid Event)
1:00PM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 802062025 NTM & Bronchiectasis Conference for Healthcare Providers (Hybrid Event)
1:00PM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 802062025 NTM & Bronchiectasis Conference for Healthcare Providers Sponsors and Exhibitors
1:00PM
Molly Blank Conference Center
1400 Jackson Street, Denver, Colorado 802062025 NTM & Bronchiectasis: Patient & Family Conference (Hybrid Event)
8:30AM
National Jewish Health - Molly Blank
1400 Jackson Street, Denver, Colorado 80206October
21st Annual Respiratory Disease Young Investigators’ Forum
8:00AM
Hotel Clio
150 Clayton Ln, Denver, Colorado 80206January
48th Annual Pulmonary and Allergy Update at Keystone
3:00PM
Keystone Conference Center
633 Tennis Club Road, Keystone, Colorado 80435